Why Switch to Fertility-Friendly Skincare?
Share
Scientists have known for decades that exposure to toxic chemicals can impact negatively on fertility[1]. One source of these toxins is the products that we put on our skin, which are proven to absorb into the body[2]. Here's a summary of what we know...
Oxidative stress
Toxin exposure can cause oxidation as well as compromising the body's antioxidant defence system. This can cause oxidative damage which is a contributing factor to infertility in both men and women[3].
The kinds of toxins responsible for oxidative damage are found in many everyday products including our skincare and have been proven to absorb through the skin reaching our internal tissues and organs and our bloodstream.
By detoxing your skincare, it is possible to reduce the level of these chemicals in the body and take a step to guard against oxidative damage.
Sperm health
It is well established that higher levels of toxins in men have been linked to lower sperm count, motility and morphology and a greater percentage of sperm DNA damage therefore significantly affecting sperm quality[4]. Oxidative stress and altered hormone levels are relevant factors here.
Egg health
Evidence has shown that high toxin levels in the body also correlate with reduced egg quality[5], again due to oxidative stress and altered hormone levels. Studies have also linked chemical toxin exposure to diminished ovarian reserve[6].
Natural conception
These kinds of chemicals can compromise the activity of hormones in both men and women that are critical for fertility. Those with high levels of toxins in their bodies are likely to find it more difficult to get pregnant[7].
IVF
Studies show higher rates of toxin exposure are associated with less mature eggs in IVF[8], reduced embryo quality[9] and lower probability of success in IVF treatment[10].
Pregnancy
Toxins have been shown to cross the placenta and have been found in both the amniotic fluid and the fetus during pregnancy[11]. A developing fetus is vulnerable to the toxic effects of such chemicals.
Miscarriage
Sadly numerous studies over the last decade have shown a link between pregnancy loss and the chemicals we are exposed to[12].
General health
Many of these types of chemicals are linked to other serious health concerns including cancer, autoimmune disease, thyroid disorder and diabetes[13].
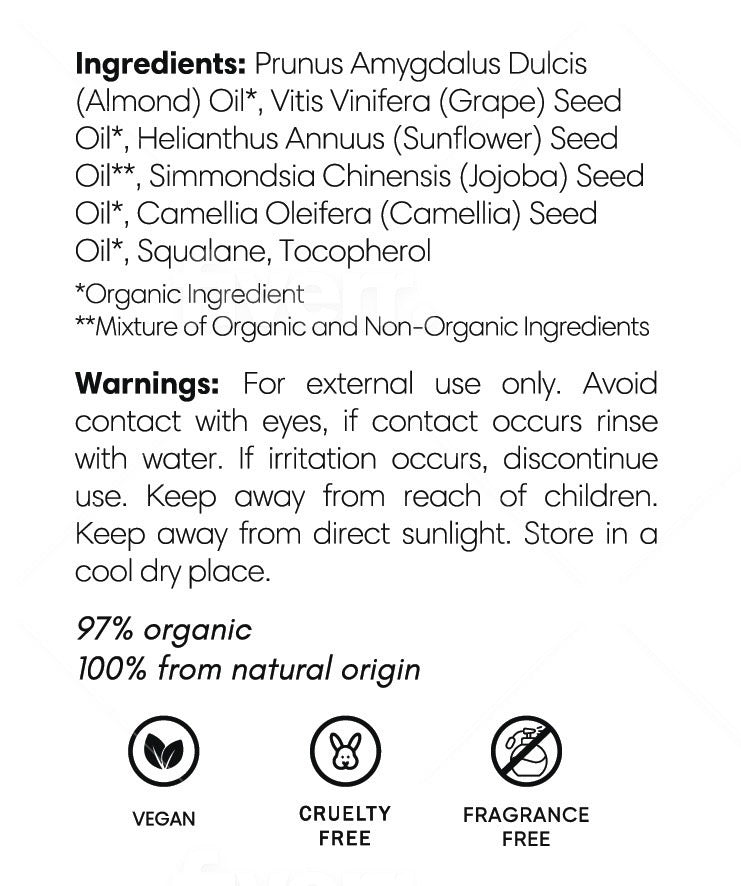
It is possible to limit toxin exposure by using nontoxic skincare and cosmetics. Switching your body oil or lotion is a good place to start as this is applied over a larger surface area of skin allowing more opportunity to be absorbed. Our hormone-safe Organic Body Oil is natural, organic, fragrance free and free of any chemical or other ingredient that could potentially impact fertility health. Also packed with natural vitamins and antioxidants, keeping your skin nourished and soft as well as giving that extra antioxidant boost to assist in combating oxidative damage.
References
[1] Duty S. M., Singh N. P., Silva M. J., Barr D. D., Brock J. W., Ryan L., Herrick R. F., Christiani D. C., Hauser R. 2003b. The relationship between environmental exposures to phthalates and DNA damage in human sperm using the neutral comet assay. Environ. Health Perspect. 111, 1164-1169. ("In conclusion, this study represents the first human data to demonstrate that urinary MEP, at environmental levels, is associated with increased DNA damage in sperm.").
[2] Wittassek M, Koch HM, Angerer J, Bruning T. Assessing exposure to phthalates - the human biomonitoring approach. Mol Nutr Food Res. 2011;55:7-31. Koniecki D, Wang R, Moody RP, Zhu J. Phthalates in cosmetic and personal care products: concentrations and possible dermal exposure. Environ Res. 2011 Apr;111(3):329-36. ("Koniecki 2011"). Janjua NR, Mortensen GK, Andersson AM, Kongshoj B, Skakkebaek NE, Wulf HC. Systemic uptake of diethyl phthalate, dibutyl phthalate, and butyl paraben following whole-body topical application and reproductive and thyroid hormone levels in humans. Environ Sci Technol. 2007 Aug 1;41(15):5564-70.
[3] Auger J, Eustache F, Andersen AG, Irvine DS, Jorgensen N, Skakkebaek NE, Suominun J, Toppari J, Vierula M, Jouannet P: Sperm morphological defects related to environment, lifestyle and medical history of 1001 male partners of pregnant women from four European cities. Hum Reprod. 2001; 16: 2710-7. Duty S. M., Singh N. P., Silva M. J., Barr D. D., Brock J. W., Ryan L., Herrick R. F., Christiani D. C., Hauser R. 2003b. The relationship between environmental exposures to phthalates and DNA damage in human sperm using the neutral comet assay. Environ. Health Perspect. 111, 1164-1169. Agarwal A, Aponte-Mellado A, Premkumar BJ, Shaman A, Gupta S. The effects of oxidative stress on female reproduction: a review. Reprod Biol Endocrinol. 2012 Jun 29;10:49. Ruder EH, Hartman TJ, Goldman MB. Impact of oxidative stress on female fertility. Curr OpinObstet Gynecol. 2009 Jun;21(3):219-22. Al-Gubory KH, Fowler PA, Garrel C. The roles of cellular reactive oxygen species, oxidative stress and antioxidants in pregnancy outcomes. Int J Biochem Cell Biol. 2010; 42:1634-1650.
[4] Armstrong JS, Rajasekaran M, Chamulitrat W, Gatti P, Hellstrom WJ, Sikka SC. Charaterization of reative oxygen species induced effects on human spermatozoa movement and energy metabolism. Free Radic. Biol. Med. 1999; 26: 869-80. 12. Kodama H, Yamaguchi R, Fukuda J, Kasai H, Tanaka T. Increased oxidative deoxyribonucleic acid damage in the spermatozoa of infertile male patients. Fertil. Steril. 1997; 68: 519-24. 13 Barroso G, Morshedi M, Oehninger S. Analysis of DNA fragmentation, plasma membrane translocation of phosphatidylserine and oxidative stress in human spermatozoa. Hum. Reprod. 000; 15: 1338-44. Mahfouz R, Sharma R, Thiyagarajan A, Kale V, Gupta S, Sabanegh E, Agarwal A. Semen characteristics and sperm DNA fragmentation in infertile men with low and high levels of seminal reactive oxygen species. Fertil Steril. 2010 Nov;94(6):2141-6. Huang XF, Li Y, Gu YH, Liu M, Xu Y, Yuan Y, Sun F, Zhang HQ, Shi HJ. The effects of Di-(2-ethylhexyl)-phthalate exposure on fertilization and embryonic development in vitro and testicular genomic mutation in vivo. PLoS One. 2012;7(11):e50465. Pant N, Pant A, Shukla M, Mathur N, Gupta Y, Saxena D. Environmental and experimental exposure of phthalate esters: the toxicological consequence on human sperm. Hum Exp Toxicol. 2011 Jun;30(6):507-14. Duty S. M., Singh N. P., Silva M. J., Barr D. B., Brock J. W., Ryan L., Herrick R. F., Christiani D. C., Hauser R. 2003b. The relationship between environmental exposures to phthalates and DNA damage in human sperm using the neutral comet assay. Environ. Health Perspect. 111, 1164-1169. ("In conclusion, this study represents the first human data to demonstrate that urinary MEP, at environmental levels, is associated with increased DNA damage in sperm.").
[5] Grossman D, Kalo D, Gendelman M, Roth X.Effect of di-(2-ethylhexyl) phthalate and mono-(2-ethylhexyl) phthalate on in vitro developmental competence of bovine oocytes. Cell Biol Toxicol. 2012 Dec;28(6):383-96. ("Grossman 2012"). Gupta RK, Singh JM, Leslie TC, Meachum S, Flaws JA, Yao HH. Di-(2-ethylhexyl) phthalate and mono-(2-ethylhexyl) phthalate inhibit growth and reduce estradiol levels of antral follicles in vitro. Toxicol Appl Pharmacol. 2010 Jan 15;242(2):224-30. ("Gupta 2010").
[6] Smith KW, Souter I, Dimitriadis I, Ehrlich S, Williams PL, Calafact AM, Hauser R. Urinary paraben concentrations and ovarian aging among women from a fertility center. Environ Health Perspect 2013 Aug;121:1299-1305.
[7] Anas MK, Suzuki C, Yoshioka K, Iwamura S. Effect of mono-(2-ethylhexyl) phthalate on bovine oocyte maturation in vitro. ReprodToxicol. 2003 May-Jun;17(3):305-10; Ambruosi B, Uranio MF, Sardanelli AM, Pocar P, Martion NA, Paternoster MS, Amati F, Dell-Aquila ME. In vitro acute exposure to DEHP affects oocyte meiotic maturation, energy and oxidative stress parameters in a large animal model. PLoS One. 2011;6(11):e27452; Grossman D, Kalo D, Gendelman M, Roth X.Effect of di-(2-ethylhexyl) phthalate and mono-(2-ethylhexyl) phthalate on in vitro developmental competence of bovine oocytes. Cell Biol Toxicol. 2012 Dec;28(6):383-96. ("Grossman 2012"). Gupta RK, Singh JM, Leslie TC, Meachum S, Flaws JA, Yao HH. Di-(2-ethylhexyl) phthalate and mono-(2-ethylhexyl) phthalate inhibit growth and reduce estradiol levels of antral follicles in vitro. Toxicol Appl Pharmacol. 2010 Jan 15;242(2):224-30. ("Gupta 2010"). Buck Louis G.M., Sundaram R., Sweeney A., Schisterman E.F., Kannan K. Bisphenol A, phthalates and couple fecundity, the life study. Fertil. Steril. 2013 Sep; 100(3): S1.
[8] Hauser R, Gaskins AJ, Souter I, et al. Urinary phthalate metabolite concentrations and reproductive outcomes among women undergoing fertilization: results from the EARTH Study. Environ Health Perspect2016;124:831-9.
[9] Hong YC, Park EY, Park MS, Ko JA, Oh SY, Kim H, Lee KH, Leem JH, Ha EH. Community level exposure to chemicals and oxidative stress in adult population. Toxicol. Lett. 2009;184(2):139-144; Ferguson KK, Loch-Caruso R, Meeker JD. Urinary phthalate metabolites in relation to biomarkers of inflammation and oxidative stress: NHANES 1999-2006. Environ Res. 2011 Jul:111(5):718-26. ("Ferguson 2011").
[10] Hauser R, Gaskins AJ, Souter I, Smith KW, Dodge LE, Ehrlich S, Meeker JD, Calafat AM, Williams PL, EARTH Study Team. Urinary phthalate metabolite concentrations and reproductive outcomes among women undergoing in vitro fertilization: results from the EARTH study. Environmental Health Perspectives. 2016 Jun 1;124(6):831.
[11] Latini G, et al. In utero exposure to di-(2-ethylhexyl)phthalate and duration of human pregnancy. Environmental Health Perspectives. 2003;111:1783-1785. Bornehag, C. G., Lindh, C., Reichenberg, A., Wikstrom, S., Hallerback, M. U. Evans, S. F.,...& Swan, S. H. (2018). Association of prenatal phthalate exposure with language development in early childhood. JAMA pediatrics, 172(12), 1169-1176.
[12] Lathi RB, Liebert CA, Brookfield KF, et al. Conjugated bisphenol A in maternal serum in relation to miscarriage risk. Fertil Steril2014;102:123-8. Krieg SA, Shahine LK, Lathi RB. Environmental exposure to endocrine-disrupting chemicals and miscarriage. Fertil Steril2016;106:941-7. Brieno-Enriquez MA, Robles P, Camats-Tarruella N, et al. Human meiotic progression and recombination are affected by bisphenol A exposure during in vitro human oocyte development. Hum Reprod2011;26:2807-18. Toft G, Jonsson BA, Lindh CH, et al. Association between pregnancy loss and urinary phthalate levels around the time of conception. Environ Health Perspect2012;120:458-63.
[13] Reddy BS, Rozati R, Reddy BV, Raman NV. Association of phthalate esters with endometriosis in Indian women. Bjog. 2006;113:515-20. Kim SH, Chun S, Jang JY, Chae HD, Kim CH, Kang BM. Increased plasma levels of phthalate esters in women with advanced-stage endometriosis: a prospective case-control study. Fertil Steril. 2011 Jan;95(1):357-9. Buck Louis GM, Peterson CM, Chen Z, Croughan M, Sundaram R, Stanford J, Varner MW, Kennedy A, Giudice L, Fujimoto VY, Sun L, Wang L, Guo Y, Kannan K. Bisphenol A and phthalates and endometriosis: the Endometriosis: Natural History, Diagnosis and Outcomes Study. Fertil Steril. 2013 Jul;100(1):162-9.el-2. Park SY, Kong SH, Kim KJ, Ahn SH, Hong N, Ha J, Lee S, Choi HS, Baek KH, Kim JE, Kim SW; Metabolic Bone Disease Study Group of Korean Endocrine Society.Endocrinol Metab (Seoul). 2024 Jul 17. doi: 10.3803/EnM.2024.1963. Benjamin S, Masai E, Kamimura N, Takahashi K, Anderson RC, Faisal PA.J Hazard Mater. 2017 Oct 15;340:360-383. Dalamaga M, Kounatidis D, Tsilingiris D, Vallianou NG, Karampela I, Psallida S, Papavassiliou AG.Int J Mol Sci. 2024 Jan 4;25(1):675. Di Donato M, Cernera G, Giovannelli P, Galasso G, Bilancio A, Migliaccio A, Castoria G.Mol Cell Endocrinol. 2017 Dec 5;457:35-42. Seralini GE, Jungers G.Toxicol Rep. 2021 Jul 31;8:1538-1557.